Abstract
Background
Aggressive large B-Cell lymphomas (LBCLs) commonly harbor genetic alterations in the p53 tumor suppressor pathway. A subgroup analysis of the RICOVER-60 trial documented p53 mutations in approximately 25% of Diffuse Large B-cell Lymphoma (DLBCL-NOS), which carried inferior overall survival (OS) and lower complete remission (CR) rates.1 Overcoming p53 resistance may be an unmet need in the treatment of DLBCL-NOS, but less is known about p53 alterations and other LBCL. High grade B-cell lymphomas (HGBL) represent a rare and poorly elucidated diagnosis with inferior treatment outcomes and unknown optimal therapy. We therefore set out to compare p53 overexpression in HGBL to other aggressive LBCL cases and evaluate its comparative prognostic impact following frontline chemoimmunotherapy (CIT).
Methods
A LBCL database was created by searching the electronic medical record for appropriate ICD-10 codes. This list was used to confirm LBCL diagnosis and in-house histopathology samples at our medical center. LBCL patients with p53 immunohistochemical (IHC) staining were included, and patients who had tissue blocks available for add-on p53 IHC were also included. For p53 evaluation, standard IHC was performed with Dako mouse monoclonal antibody against p53 (clone DO-7). Cases were considered positive if the lymphoma cells showed >10% strong expression or >20% intermediate expression compared to a positive control. Patients received combination CIT in accordance with widely accepted standard of care regimens. Patient information collected included demographics (age, sex, race), WHO diagnosis, stage, IPI score, IHC protein expression, treatment and clinical outcomes. Data were summarized with descriptive statistics. Patient characteristics were compared between the groups using two-sample t-tests and chi-square tests. Outcomes were examined using Kaplan Meier curves and log-rank test. Time to events (PFS, OS) were modeled using Cox Proportional Hazards models.
Results
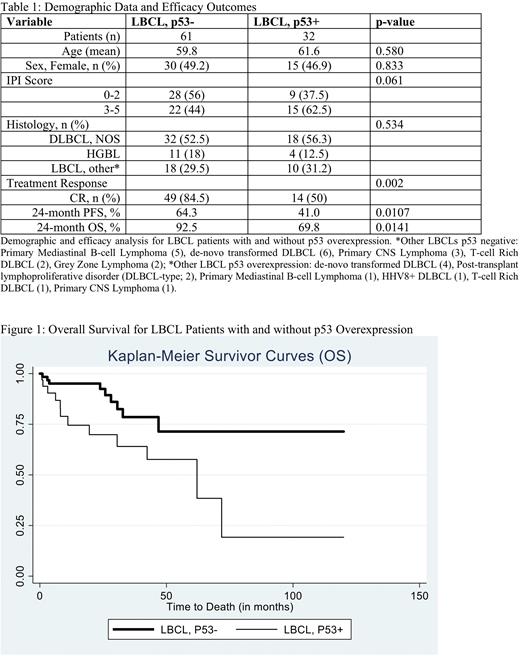
We identified 93 newly diagnosed LBCL cases at our center where p53 IHC was successfully performed. Demographic data is depicted in Table 1; patients mean age was approximately 60 years, most patients presented with advanced stage (66.7% vs 73.3%, p = 0.958) and 44% of the p53 negative cohort was IPI score 3-5, compared to 62.5% of the p53 overexpression cohort (p =0.061). Cases included in the analysis had a diagnosis of DLBCL-NOS (50 [53.8%]), HGBL (15 [16.1%]), or other LBCL (28 [30.1%]). P53 overexpression was reported in 32 (34.4%) of 93 patients overall - this included 18 (56.3%) of DLBCL-NOS, 4 (12.5%) of HGBL and 10 (31.2%) other LBCL. Histology was balanced equally in each LBCL cohort (p = 0.534).
Overall CR and partial remission (PR) rates for all 93 patients were 73.3% and 16.3% respectively. 84.5% of patients in the LBCL p53 negative cohort achieved a CR to initial CIT, compared to 50% of the p53 overexpression group (p = 0.002). 31.0% of the p53 negative cohort was documented to have primary refractory or relapsed disease, compared to 53.6% of the p53 overexpression group (p = 0.009). Estimated 24-month progression free survival (PFS) was 64.3% compared to 41.0% (p = 0.0107, HR 2.12, 95% CI 1.17 - 3.84, p = 0.013) and 24-month overall survival (OS) was 92.5% versus 69.8% (p = 0.0141; HR 2.82, 95% CI 1.18 - 6.71, p = 0.019) in the p53 negative versus p53 overexpression patients. Figure 1 highlights the overall survival between the two cohorts. Subgroup analysis of the HGBL and DLBCL, NOS patients was comparable to the full dataset; CR rates (89.7% vs 47.4%; p = 0.001) refractory/relapsed disease (33.3% vs 63.2%, p = 0.014), 24-month PFS (60.4% vs 33.8%, p = 0.014) and 24-month OS (89.2% vs 60.4%, p = 0.026) all favored the p53 negative cohort. Of HGBL patients, PFS for p53 negative patients was 63.6% compared to 33.3% for the p53 overexpression cohort.
Conclusion
In a single-center experience of 93 newly diagnosed LBCL patients, we found 34% to overexpressed p53, with these patients experiencing inferior OS, PFS and CR rates. P53 overexpression and clinical outcomes were similar among HGBL, DLBCL-NOS and other LBCL histologies. P53 IHC is a rapid and cost-effective diagnostic tool for prognostication in LBCLs including HGBL. P53 IHC analysis should be routinely performed in the assessment of HGBL and other LBCLs as its role in conjunction with other molecular and clinical factors continues to be investigated in clinical trials.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal